Abstract
Objective: Adult scoliosis (AS) is often associated with rotational thoracolumbar (TL) kyphosis. The impact of surgical correction on lumbar sagittal distribution, ideal sagittal plane matching, and mechanical complications is still underexplored.
Methods: In this retrospective study, prospectively collected data were analyzed from a multicenter adult deformity database. Inclusion criteria were surgical patients with AS and TL/L curves > 30°, T10-L2 sagittal kyphosis (TLK) > 20°, and at least a 2-year follow-up. We analyzed preoperative and postoperative variables and studied the consequences of TL sagittal change on ideal type mismatch and on mechanical complications using univariate and multivariate logistic regression analyses, and compared patients with high pelvic incidence (PI > 50°) versus those with low PI (PI < 50°).
Results: A total of 171 patients were included. The TLK segment flattened by a mean of 20° after surgery. The residual TLK kyphosis matched that expected by PI. The TL sagittal change was not directly associated with complications or ideal shape mismatch.
Mechanical complications were associated only with older age and pelvic instrumentation. Patients with low and high PI were found to have similar Cobb angle correction, TLK correction, and rate of mechanical complications. However, it was more challenging to restore an ideal sagittal profile in patients with high PI and in patients fused to the pelvis.
Conclusions: Surgical correction of adult TL scoliosis flattens the TL segment by about 20°, automatically adjusting to the ideal parameters dictated by patients’ PI. The TL segment change lengthens the upper lumbar arc by one segment, shifting the inflection point cranially. However, this change has no direct impact on mechanical complications or final sagittal shape matching.Resumen
Objetivos: La escoliosis del adulto asocia con frecuencia una cifosis toracolumbar (TL) rotacional. Desconocemos el efecto que produce su corrección quirúrgica con respecto a la distribución de la lordosis, el ajuste con el plano sagital ideal y las complicaciones mecánicas.
Métodos: Análisis retrospectivo de datos recogidos de manera prospectiva de una base de datos de deformidad del adulto. Incluimos pacientes tratados quirúrgicamente por curvas TL/lumbares > 30°, con cifosis T10-L2 (CTL) > 20° y al menos dos años de seguimiento. Analizamos variables preoperatorias y postoperatorias, estudiando las consecuencias derivadas del cambio sagital del segmento TL con respecto al desajuste del tipo sagital ideal y a las complicaciones mecánicas usando análisis univariante y multivariante de regresión logística. Comparamos pacientes con incidencia pélvica alta (PI > 50°) vs baja (PI < 50°).
Resultados: Incluimos 171 pacientes. El segmento de CTL se aplanaba una media de 20° con la cirugía. La cifosis TL residual se ajustaba a la ideal esperada por la Incidencia Pélvica. Este cambio sagital TL no se asociaba directamente a complicaciones o al desajuste del perfil ideal.
Las complicaciones mecánicas sólo se asociaban a mayor edad e instrumentación hasta la pelvis. Comparando pacientes con PI alta y baja la corrección del Cobb fue similar, al igual que la corrección de la CTL y el porcentaje de complicaciones mecánicas. Resultó más difícil restaurar el plano sagital ideal en pacientes con PI-alta y aquellos fusionados a la pelvis.
Conclusiones: La corrección quirúrgica de la escoliosis TL aplana el segmento TL unos 20°, automáticamente ajustándose a los parámetros dictados por la incidencia pélvica. Este cambio TL alarga el arco lumbar superior en un segmento, trasladando el punto de inflexión a craneal. Sin embargo, este cambio no tuvo un impacto directo en las complicaciones mecánicas o el ajuste final del perfil sagital.Keywords: Adult Scoliosis; Scoliosis Correction; Sagittal Plane; Thoracolumbar Kyphosis; Lordosis Distribution; Mechanical Complications.
Palabras clave: Escoliosis del Adulto; Corrección de la Escoliosis; Plano Sagital; Cifosis Toracolumbar; Distribución de la Lordosis; Complicaciones Mecánicas.
INTRODUCTION
In the past decade, there has been increasing interest in the study of adult spinal deformity. Patients with this condition may have pain, disability, mental health problems, and concerns about their physical appearance. Surgery has been demonstrated to be effective in treating spinal deformity. Controlling both coronal and sagittal deformity and addressing the degenerative changes that cause pain can relieve symptoms and improve patient reported outcome measures. Sagittal plane correction has been the focus of much study, as it seems to be the most influential parameter on clinical symptoms. Surgical planning should aim to restore sagittal balance and the ideal parameters of healthy individuals.
Thoracolumbar (TL) scoliosis is often associated with rotational or transitional thoracolumbar kyphosis (TLK). When the apex of the coronal curve is located at the thoracolumbar junction, the rotation created by the axial plane deformity often draws a false kyphosis at this segment, as seen on plain lateral radiograph [1]. The surgical correction of scoliosis in one plane leads to correction of the other planes by coupling effect [2]. Thus, when translating the coronal plane and derotating the axial plane, the sagittal plane automatically flattens [3]. This rotational kyphosis decrease at the TL junction should produce lordosis at the upper lumbar arc, migration of the inflexion point to a more cranial location, and should add more vertebrae into the global lordosis [4], eventually modifying the preexisting lordosis distribution [5].
The sagittal plane of healthy adults varies by pelvic anatomy and sacral inclination [6, 7]. We know that adult scoliosis (AS) can distort the ideal sagittal profile [8], and one of the goals of surgery should be to restore the proper sagittal shape and lumbar distribution to prevent mechanical complications [9]. Typical mechanical complications are rod breakage due to pseudoarthrosis, proximal junctional kyphosis and screw pull-out or loosening.
Little is known about the role of TLK in this process. What impact does surgery have on the sagittal profile of patients with scoliosis who have TL rotational kyphosis? How much does this change affect the sagittal plane matching its ideal type and the outcome in terms of mechanical failure? Do results differ when flattening the upper lumbar arch between patients with low vs high pelvic incidence (PI)?
The aim of our study was to analyze a cohort of adult surgical patients with scoliosis and thoracolumbar rotational kyphosis, to understand how the lateral projection of this segment changes after surgery, what impact this change has on lumbar sagittal distribution and ideal sagittal plane matching, and its consequences on mechanical complications.
MATERIAL AND METHODS
We conducted a retrospective analysis of prospectively collected data from a multicenter adult deformity database European Spine Study Group (EESG). Database enrollment criteria were age ≥ 18 years and at least 1 of the following: coronal Cobb angle of ≥ 20°, sagittal vertical axis of ≥ 5 cm, pelvic tilt of ≥ 25°, and thoracic kyphosis of ≥ 60°. Institutional review board approval was obtained at each site for patient enrollment and data collection protocols. All patients signed an informed consent prior to enrollment.
The inclusion criteria for this specific study were surgical patients with AS and a TL/L curve > 30° (double or single TL/L curves), T10-L2 sagittal kyphosis defined as (TLK) > 20°, and at least a 2-year follow-up.
We analyzed the following preoperative and 2-year postoperative coronal and sagittal radiographic parameters: coronal TL Cobb angle, TL coronal translation (measured from the TL coronal apex to the central sacral vertical line), thoracolumbar kyphosis (TLK) (T10-L2), maximal lumbar lordosis (MaxLL) (measured from the inflection point to S1 endplate), pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), inflection point (where kyphosis transitions to lordosis) [5], type of Roussouly sagittal shape (R-type), and the location of the upper and lower instrumented vertebra (UIV and LIV).
Postoperative SS dictated the type of postoperative Roussouly sagittal shape (R-type 1 and 2, SS < 35°; R-type 3, SS = 35°-45°; R-type 4, SS > 45°) [6]. Preoperative PI dictated the ideal sagittal shape (R-type 1 and 2, PI < 45°; R-type 3, PI = 45°-60°; R-type 4, PI > 60°) [7]. Sagittal type matching was calculated from the difference between ideal type and postoperative type.
We investigated the assocaition between these variables and postoperative ideal type mismatch and mechanical complications (proximal junctional kyphosis or failure, rod breakage and screw failure), placing special focus on the consequences of TL sagittal change. We also compared results in patients with high-PI (PI > 50°) and patients with low-PI (PI < 50°).
The statistical analysis was performed with SPSS version 20 (SAS Institute Inc., Cary, NC, USA). The distribution of variables were expressed as mean and standard deviation. Normal distribution of the variables was evaluated using Kolmogorov-Smirnov test. Univariate analysis was performed comparing qualitative variables using chi-square statistics (and Fisher test when necessary), and quantitative variables using the Student-t test or analysis of variance (ANOVA) with Bonferroni correction. Multivariate logistic regression analysis was performed to identify independent factors associated with mechanical complications and sagittal shape matching. The significance threshold was set at 5% (P < 0.05).
RESULTS
Sample description
At the time of data extraction (July 2020), the database contained 1217 operated patients, 574 of whom had a scoliosis with a main coronal TL/L curve > 30°. Of these patients, 185 (32%) fulfilled the T10-L2 kyphosis > 20° criterion and 171 had at least 2 years of follow-up. Our study cohort therefore comprised 171 patients.
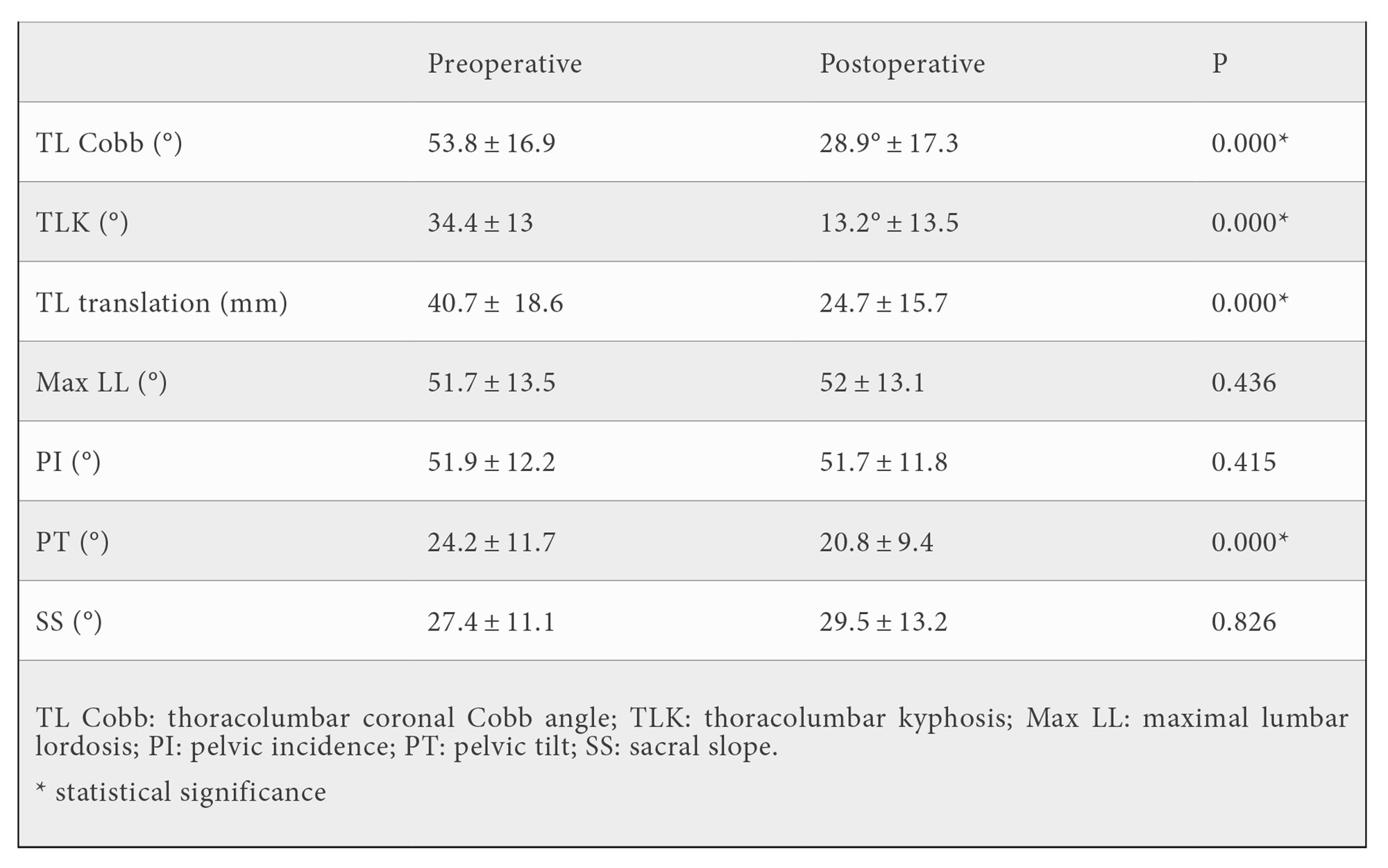
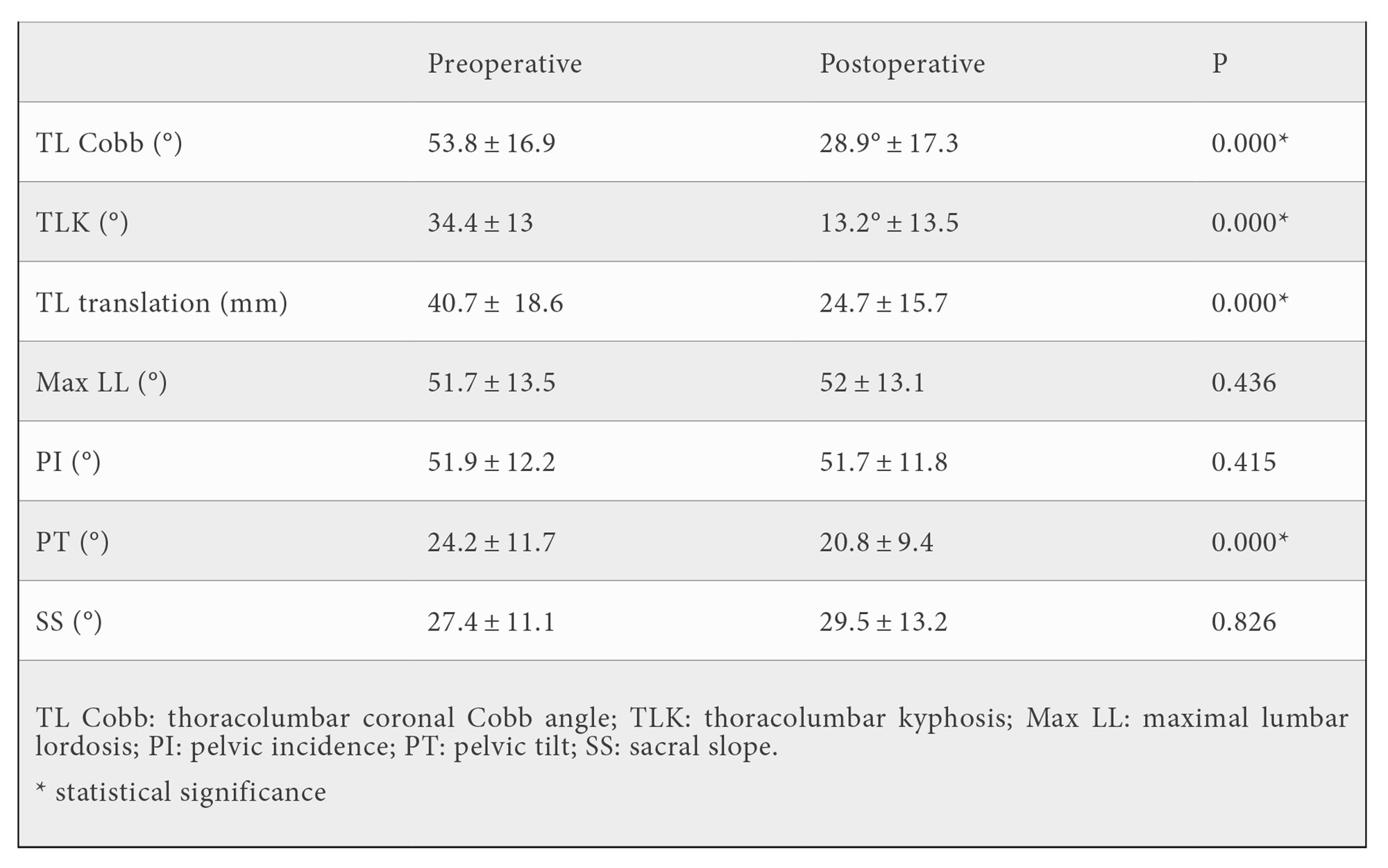
The mean age was 57.8 ± 14.8 years, mean preoperative TL Cobb angle was 53.8 ± 16.9°, and preoperative TLK was 34.4 ± 13° (Table 1). The LIV was the pelvis in 48.6% of the patients and 51.4% were instrumented at L5 or above (15.5% at L5, 28.4% at L4, 7.4% at L3). The UIV was between T2-T6 in 49.7% of the patients, and between T7-T10 in 50.3% of them. Surgery achieved a TLK mean correction of 21.4 ± 18.1°. This shifted the inflection point to a higher position by a mean of 1.4 ± 1.25 segments.
Mechanical complications
Postoperative mechanical complications were found in 38% of the patients (Table 2).
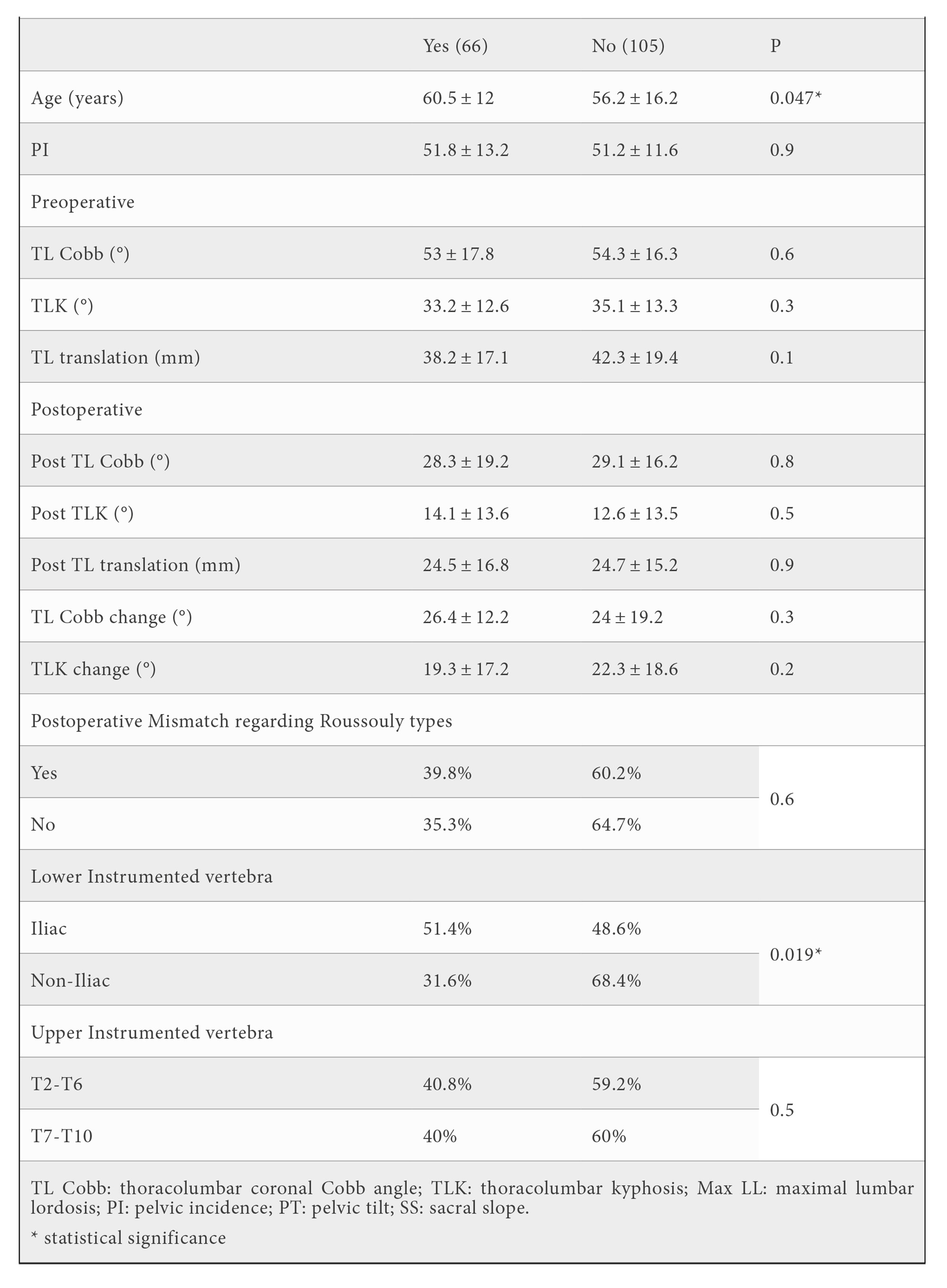
The univariate analysis showed that older patients as well as those instrumented to the pelvis (iliac) were statistically more prone to have mechanical complications. However, the difference in age did not appear to be clinically relevant (60.5 ± 12 vs 56.2 ± 16.2 years) and multivariate analysis did not show independent factors associated with mechanical complications. We were not able to identify any other studied parameter associated with mechanical complications (coronal Cobb, TL translation, or UIV). In fact, neither preoperative TLK nor TLK change after surgery seemed to influence mechanical complications. There was no difference in the rate of mechanical complications when comparing patients with low PI (PI < 50°) whose TLK remained postoperatively above 20° with those whose TLK was corrected to below 20°.
High PI vs low PI
When comparing patients with high PI and those with low PI (Table 3), we found that those with high PI had greater postoperative MaxLL (56.3 ± 12.4° vs 47.1 ± 11.7°) as well as a flatter TLK (9.9 ± 10.5° vs 17.2 ± 15.7°), P = 0.002; which match the expected parameters as per ideal sagittal shape. However, patients with high PI also had a higher rate of postoperative sagittal type mismatch (76.2% vs 28.4%; P < 0.001) for postoperative SS not meeting the ideal values. Despite this fact, we were unable to find differences between the high and low PI groups regarding mechanical complications (37.5% and 39.7%, respectively) or TLK correction (23.1° and 19.7° change, respectively).
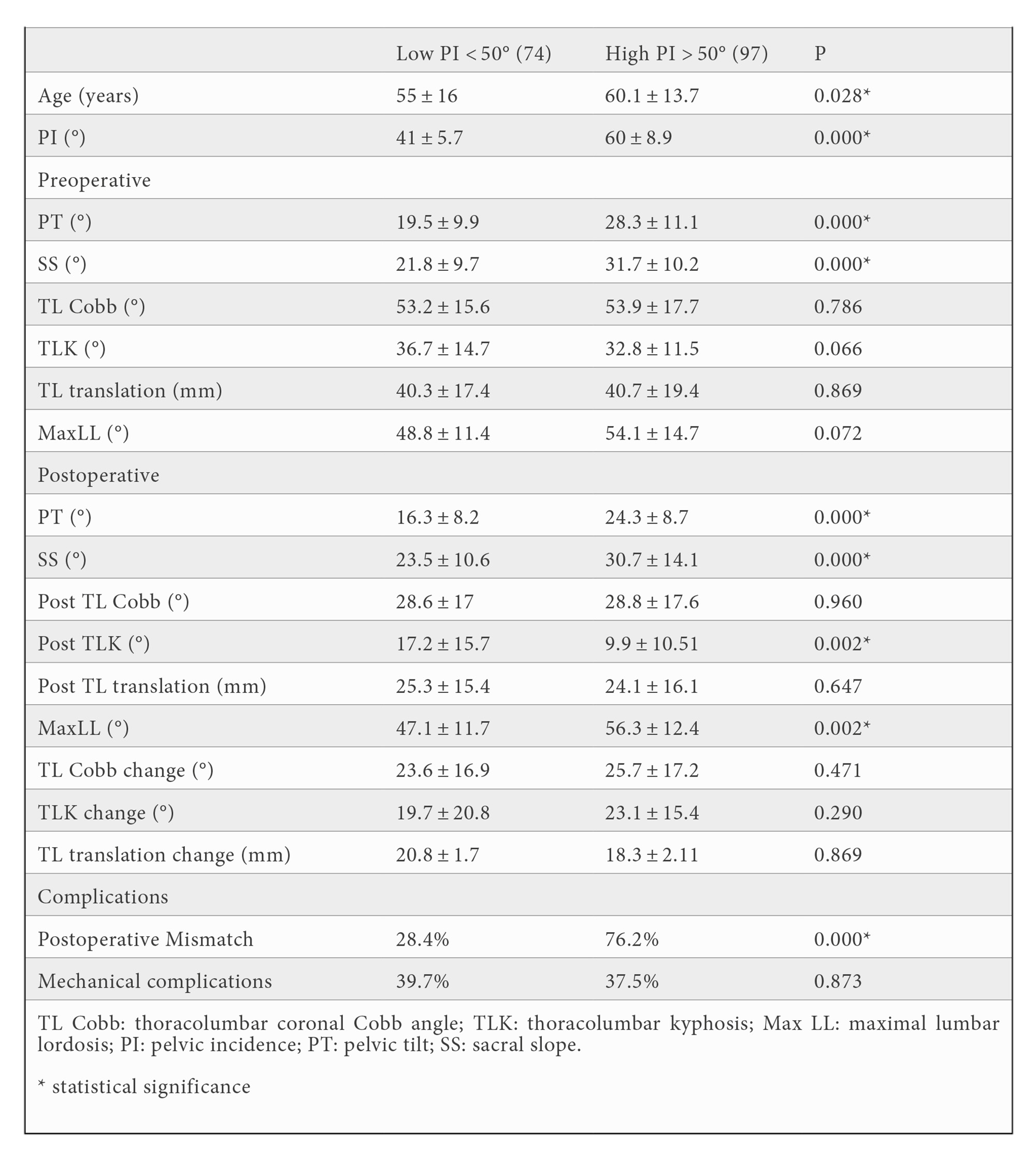
Sagittal plane mismatch
Patients instrumented to the pelvis had a higher rate of mismatch (65.1%) compared to those whose LIV was above the sacrum (47%), P = 0.029. Matching was more easily achieved in patients with LIV at L4 compared to those instrumented to the pelvis. The multivariate analysis showed that PI [OR = 0.92 (95% CI = 0.85-0.99; P = 0.046)] was the most important, and the only independent factor related to mismatch (there was 3.2 times more risk of mismatching if when PI > 50°). The usual mismatch resulted from recreating a “lower” Roussouly type than ideal. Mismatched lower R-types had lower postoperative TLK, and mismatched higher R-types had higher postoperative TLK. However these differences were not statistically significant. The mechanical complication rate was the same in all R-types (Table 4).
DISCUSSION
Scoliosis consists of the abnormal shape of the spine in the three spatial planes. In the coronal plane there is lateral deviation; in the sagittal plane, an inversion of the physiological curves; and in the axial plane, rotation. The goal of surgery is to improve the deformity in all three planes. The sagittal plane is the most important when assessing adult deformity. Sagittal malalignment has been associated with worse clinical symptoms. For this reason, restoring the sagittal plane to its ideal values and position is crucial in spinal deformity surgery. Bringing back normal alignment improves patients’ quality of life, mainly in terms of pain and disability, and reduces the risk of mechanical complications (rod breakage, proximal junctional kyphosis or screw failure) [9].
Roussouly [6] described a classification of 4 different sagittal shapes (R-types), based on sacral slope values, in an asymptomatic adult population. As sacral slope is modified by the degenerative loss of lumbar lordosis, a renewed classification [7] distributes sagittal shapes according to pelvic incidence values, which are considered to be constant throughout life. Patients with low PI (R-type 1) ideally have a short lumbar lordosis with an inflection point at L3, followed by a large TL kyphosis, since this segment belongs to the lower thoracic arc. At the other end of the spectrum, patients with high PI (R-type 4) have a long lordosis, ending at the inflection point located around T12, with a long upper lumbar arc that contains the TL segment, drawing a flattened sagittal shape at the TL transition. It is important to be aware of these parameters when planning the surgery for ideal sagittal plane restoration. However, the role of the deformity created by scoliosis at the thoracolumbar junction is still not well understood, particularly how modifying its shape affects the surgical outcome.
In one third of patients with AS, the 3D configuration of the deformity modifies this ideal sagittal shape [8]. In particular, the axial rotation of the apical segment, usually located at the thoracolumbar junction, creates a rotational thoracolumbar kyphosis when seen in a lateral view. This makes “higher” types of sagittal configuration (R-types 3 and 4) resemble “lower” types (mainly R-type 1). Thus, greater rotational T10-L2 kyphosis means the lumbar spine has fewer vertebrae involved in the lordosis, leading to a caudal shift in the inflection point, and increasing the lordosis distribution index, resembling a R-type 1-like sagittal shape.
After analyzing a large cohort of adult surgical scoliosis patients with thoracolumbar curves in our database, we discovered that TL kyphosis is relevant (above 20°) in only one third of these patients. The patients we studied had moderate coronal TL deformity (53°) and a pronounced mean TL kyphosis (34°) with a narrow range across the different R-types. The purpose of this study was to identify to what extent this TL rotational kyphosis was corrected by surgery, and the possible consequences of correcting TL rotational kyphosis in terms of final ideal R-type restoration and mechanical complications. It is widely believed that proper sagittal shape must be restored with surgery to obtain the best outcomes, because achieving ideal alignment and lordosis distribution may help avoid postoperative mechanical complications [4, 10-12]. One of the main causes of mechanical problems is over flattening of the upper lumbar arc in patients that need some TLK in this segment, typically among patients with low PI [4].
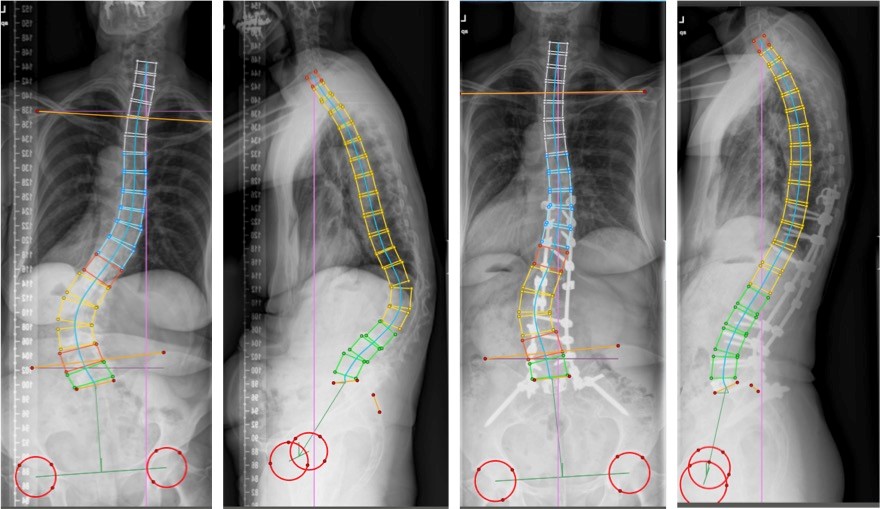
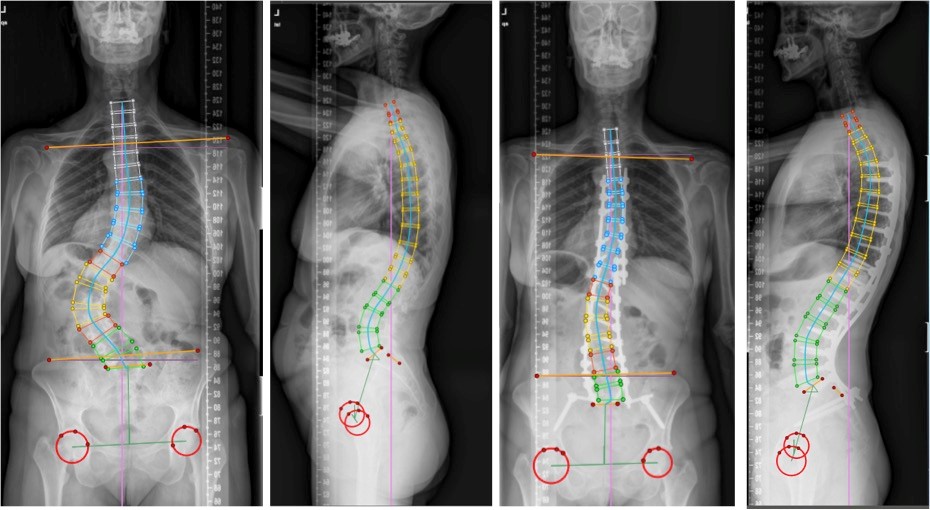
We found that the combination of maneuvers performed in scoliosis surgical correction automatically flattened the TL segment viewed from the lateral plane, changing the residual transitional kyphosis. This residual TL kyphosis readily accommodated the ideal values dictated by ideal sagittal shape configuration (Figure 1 and 2). Thus, although the degree of correction was similar regardless of PI (approximately 20°, ranging from 19° to 23°), patients with low PI ended up with higher residual TL kyphosis (17°), while patients with high PI had a flatter residual TL transition (9°). The postoperative range for maximal lordosis closely followed the ideal for each PI value (ranging from 47° for low PI to 56° for high PI). Scoliosis surgical correction also lengthened the upper lumbar arc by including a mean of one vertebra more in the lordosis, shifting the inflection point one segment towards a more proximal position.
However, we found that the change in TL kyphosis did not have a direct impact on final shape matching, whereas fusion to pelvis and especially PI did. Restoring the sagittal plane to match its ideal does not exclusively depend on the amount of kyphosis or length of TL segment, but also, and mainly, on the value of the sacral slope related to the value of pelvic incidence (relative pelvic version [12]). Fusing distally to a more proximal level leaves some room for compensation to occur in the unfused distal segments, while the alternative (fusion to pelvis) does not. Fusing to the pelvis allows only small deviations from the ideal shape, and forces surgeons to be as accurate as possible in the restoration of the SS. Indeed, most of the mismatches were caused by not achieving an adequate SS in patients with high PI (as they need higher SS values and this failed to be achieved). On the other hand, mismatching in patients with low PI resulted from overcorrecting the SS.
Changes in TLK from surgery did not seem to have a direct impact on mechanical complications, although theoretically the TL transition can lead to anchor failure and junctional kyphosis when instrumentation ends at this transition. No differences in terms of mechanical complications were found between patients instrumented to the upper vs lower thoracic spine. Over one third of our patients had mechanical complications, all of which were associated with older age and instrumentation to pelvis. Pelvic incidence, sagittal plane matching and TLK correction showed no impact on mechanical complications. The difference between this study and others that report a higher rate of mechanical complications in mismatched patients [10, 13] may be due to the fact that patients in this study mainly had coronal deformity and were well aligned pre- and postoperatively in terms of the sagittal plane. Another key factor is age, since patients with AS are usually younger than patients with sagittal disorders, less likely to receive pelvis instrumentation, and have more segments to compensate.
Our study as some limitations. Establishing a 20° threshold could be considered as strong evidence of TL transitional kyphosis. The threshold was based on the Lenke classification principles [14], where this degree of transitional kyphosis is considered as a criterion for curve structurality. In addition, not all TL coronal curves exhibit a kyphotic TL transition. This type of transition was found in only one third of our cohort. Therefore, the study results apply only to this specific group of patients. Lastly, although some univariate analyses showed strong associations between some variables and their relation to complications, multivariate analysis later showed confounding associations mainly concerning age and pelvic fixation, so this result should be taken with caution. Despite these limitations, the large sample size of homogeneous patients taken from a multicenter register allows for clear evidence based on robust data.
CONCLUSIONS
The surgical correction of adult TL scoliosis flattens the TL segment by about 20°, changing the residual transitional kyphosis that readily accommodates to the ideal values dictated by patients’ PI. This surgical correction lengthens the upper lumbar arc by one segment, shifting the inflection point towards a more proximal position. This change in TL kyphosis did not have any direct impact on mechanical complications or final shape matching.
FUNDING
The EESG study group receives funding from DePuy-Synthes Spine and Medtronic.
ETHICS COMMITTEE
All patients signed an informed consent to enter the study. The study was approved by the ethics committees of all recruiting sites.
BIBLIOGRAPHY
- Peloux J du, Fauchet R, Faucon B et al. The plan of choice for the radiologic examination of kyphoscolioses. Rev Chir Orthop reparatrice Appar Mot. 1965; 51: 517-524.
- Luk KD, Vidyadhara S, Lu DS et al. Coupling between sagittal and frontal plane deformity correction in idiopathic thoracic scoliosis and its relationship with postoperative sagittal alignment. Spine. 2010; 35(11): 1158-1164. doi: 10.1097/BRS.0b013e3181bb49f3
- Watanabe K, Nakamura T, Iwanami A et al. Vertebral derotation in adolescent idiopathic scoliosis causes hypokyphosis of the thoracic spine. BMC Musculoskelet Disord. 2012; 13: 99. doi: 10.1186/1471-2474-13-99
- Scemama C, Laouissat F, Abelin-Genevois K et al. Surgical treatment of thoraco-lumbar kyphosis (TLK) associated with low pelvic incidence. Eur Spine J. 2017; 26: 2146-2152. doi: 10.1007/s00586-017-4984-z
- Berthonnaud E, Dimnet J, Roussouly P et al. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005; 18: 40-47. doi: 10.1097/01.bsd.0000117542.88865.77
- Roussouly P, Gollogly S, Berthonnaud E et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005; 30: 346-353. doi: 10.1097/01.brs.0000152379.54463.65
- Laouissat F, Sebaaly A, Gehrchen M et al. Classification of normal sagittal spine alignment: Refounding the Roussouly classification. Eur Spine J. 2018; 27(8): 2002-2011. doi: 10.1007/s00586-017-5111-x
- Pizones J, Martin MB, Pérez-Grueso FJS et al. Impact of adult scoliosis on Roussouly’s sagittal shape classification. Spine. 2019; 44(4): 270-279. doi: 10.1097/BRS.0000000000002800
- Pizones J, Moreno-Manzanaro L, Sánchez Pérez-Grueso FJ et al. Restoring the ideal Roussouly sagittal profile in adult scoliosis surgery decreases the risk of mechanical complications. Eur Spine J. 2020; 29(1): 54-62. doi: 10.1007/s00586-019-06176-x
- Sebaaly A, Riouallon G, Obeid I et al. Proximal junctional kyphosis in adult scoliosis: Comparison of four radiological predictor models. Eur Spine J. 2018; 27: 613-621. doi: 10.1007/s00586-017-5172-x
- Barrey C, Darnis A. Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop. 2015; 6: 117-126. doi: 10.5312/wjo.v6.i1.117
- Yilgor C, Sogunmez N, Boissière L et al. Global Alignment and proportion (GAP) score. J Bone Joint Surg. 2017; 99: 1661-1672. doi: 10.2106/JBJS.16.01594
- Sebaaly A, Gehrchen M, Silvestre C et al. Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J. 2020; 29(4): 904-913. doi: 10.1007/s00586-019-06253-1
- Lenke LG, Betz RR, Harms J et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg. 2001; 83: 1169-1181.
CONFLICT OF INTEREST STATEMENT
The authors of this article declare that they have no conflict of interest with respect to what is expressed in this work.
Javier Pizones
Departamento de Cirugía Ortopédica y Traumatología, Hospital La Paz.
Paseo de la Castellana, 261 · 28046. Madrid, Spain.
Tlf.: +34 616 644 876 | E-Mail: javierpizones@gmail.com
Año 2022 · número 139 (02) · páginas 184 a 193
Enviado: 26.04.22
Revisado: 30.04.22
Aceptado: 14.05.22


